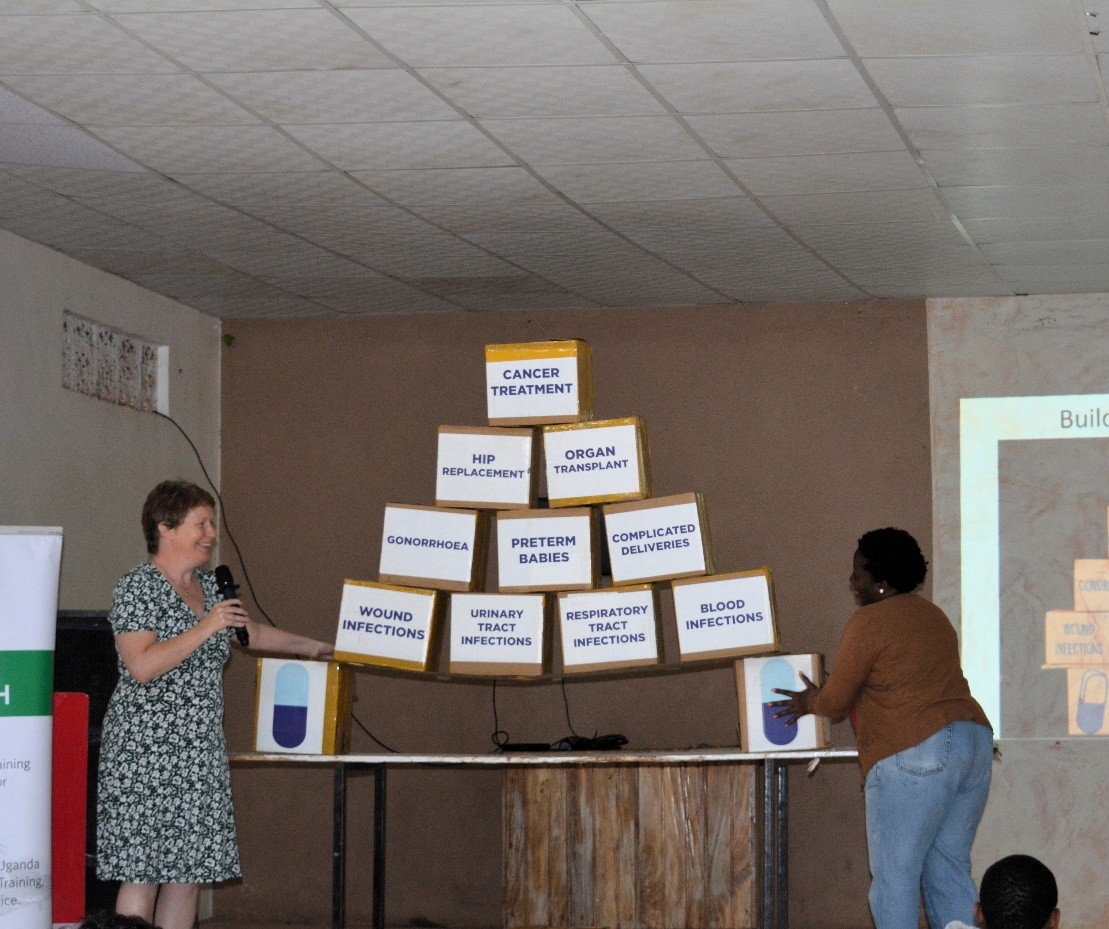
Antimicrobial resistance (AMR) is no longer a distant threat in Uganda, it is already altering how healthcare is delivered. In hospitals, clinics, and veterinary centres, frontline professionals face daily decisions on whether to prescribe antibiotics without rapid diagnostics, and how to manage infections when treatment options fail. These quick decisions, made in a flash, carry far-reaching consequences for communities, affecting human, animal, and environmental health.
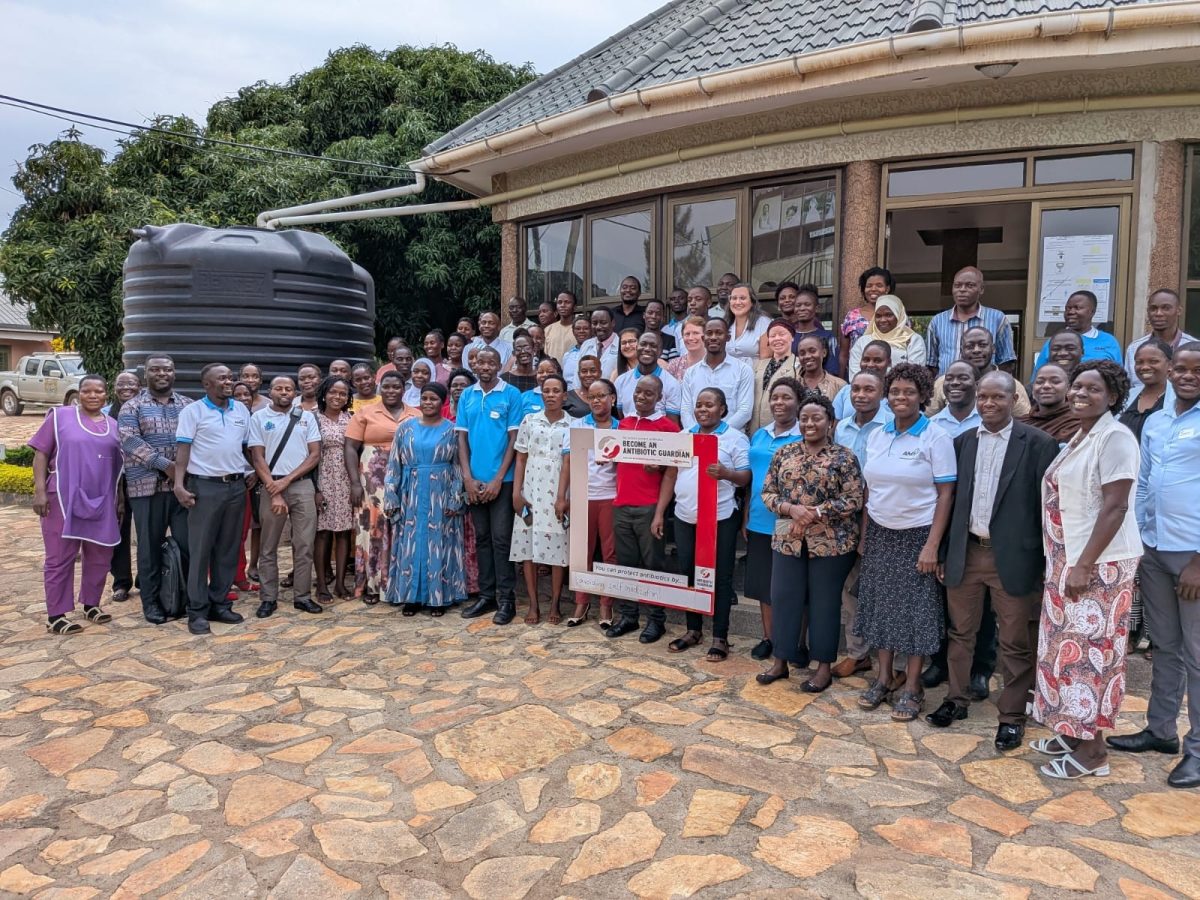
In central Uganda, a partnership between Makerere University School of Public Health (MakSPH), Nottingham Trent University (NTU), and Buckinghamshire Healthcare NHS Trust (BHT), supported by the Commonwealth Partnerships for Antimicrobial Stewardship (CwPAMS), is changing prescribing culture from reactive to deliberate. From 22–25 July 2025, the intervention, through the Centre of Excellence on Antimicrobial Stewardship (AMS) in Central Uganda, conducted a four-day training in Nakaseke and Butambala districts, targeting human, animal, and environmental health professionals.
Through the training, over 116 participants, 63 from Nakaseke and 53 from Butambala, drawn from district health teams, veterinary services, environmental health offices, and other frontline roles, engaged in interactive sessions covering Uganda’s AMR burden, the WHO AMS competency framework, AWaRe antibiotic categorisation, One Health principles, and case-based problem-solving. Practical activities such as the Glo-Germ demonstration reinforced infection prevention skills, while discussions on gender equality and social inclusion addressed equity in AMS implementation. The training also launched a Community of Practice to sustain collaboration.
The initiative’s strength lay in applied problem-solving. Reflecting on the training, Dr. David Musoke, the Uganda Project Lead, noted that participants worked through real cases from their wards, farms, and communities, testing how stewardship guidelines apply under local constraints. “They received practical tools, including the Uganda Clinical Guidelines and the Prescribing Companion App, to help embed stewardship into daily routines. The sessions went beyond prescribing to address infection prevention, hand hygiene, and the detection of substandard or falsified medicines, recognising that AMR is as much about preventing infections as treating them.”
Through our partnership with UK institutions, volunteers from the United Kingdom supported the training by sharing expertise and practical experience alongside local professionals and facilitators. This collaborative model enriched learning and reinforced the One Health approach to addressing Uganda’s AMR burden. Training outcomes underscored the need for veterinary officers to reduce antibiotic misuse in livestock to prevent resistant bacteria from entering the food chain and for clinicians and pharmacists to follow national guidelines, resist pressure to prescribe without evidence, and build patient trust. By bringing these groups together, the initiative strengthened the cross-sector coordination long missing in Uganda’s AMR response.
Equity was embedded in the discussion, facilitated by Elma Banyen, a PhD student at NTU. This session in particular emphasised how gender and socio-economic disparities influence who gets timely treatment, who can afford quality medicines, and who can demand proper care. Hence, by addressing these dynamics, especially the role of women in smallholder farming and the barriers faced by persons with disabilities, the training ensured that stewardship practices are inclusive and socially responsive.
From the participatory two-day trainings for each of the two districts of Butambala and Nakaseke, impact is already visible. Participants left with action plans to embed stewardship principles in their workplaces, ranging from ward-level prescription reviews and stronger infection prevention and control committees to community dialogues on prudent antibiotic use. In Nakaseke Hospital, the strengthened AMS committee went on to win the 2025 Antibiotic Guardian Award for infection prevention and control from the partnership, proving what’s possible when stewardship becomes part of institutional culture.

Long-term change depends on making antimicrobial stewardship a routine, though. As more facilities adopt consistent practices that encompass tracking antibiotic use, reviewing prescriptions, and involving pharmacists and veterinary officers in treatment planning, the result will be fewer unnecessary prescriptions and preserved drug effectiveness. The online Community of Practice on AMR will keep the practitioners connected, sharing updates, research, and innovations that reinforce stewardship as a shared responsibility.
This initiative, implemented in central Uganda, supports Uganda’s National Action Plan on AMR, which prioritises surveillance, stewardship, and public awareness. By building skills, providing tools, and connecting practitioners to peer networks, it turns policy into practice. Every clinician who avoids an unnecessary antibiotic, every veterinary officer who advises farmers on responsible animal treatment, and every health worker who flags a falsified medicine contributes to shifting the balance in favour of preserving vital drugs.
In the region, that shift is underway, driven by knowledge, reinforced by peer accountability, and anchored in cross-sector collaboration, through the Mak-NTU-BHT partnership’s Centre of Excellence on Antimicrobial Stewardship in Central Uganda.