Although men still face challenges in testing for HIV, a recent report shows that providing them with pre-test counseling can boost their confidence to self-test for HIV.
Researchers in the latest study entitled, “Ease of understanding and performing HIV self-tests by pregnant women and their male partners in Uganda: a cross-sectional study”, published in the International Journal of STD & AIDS have recommended furtherance of male-targeted HIV Self-Testing promotional messages to increase the involvement of Ugandan men.
This was after analysis of data on pregnant women and their partners to assess how easy it was for them to follow HIV self-testing instructions (as contained in the HIV self-test kit package) and perform the self-test unsupported.
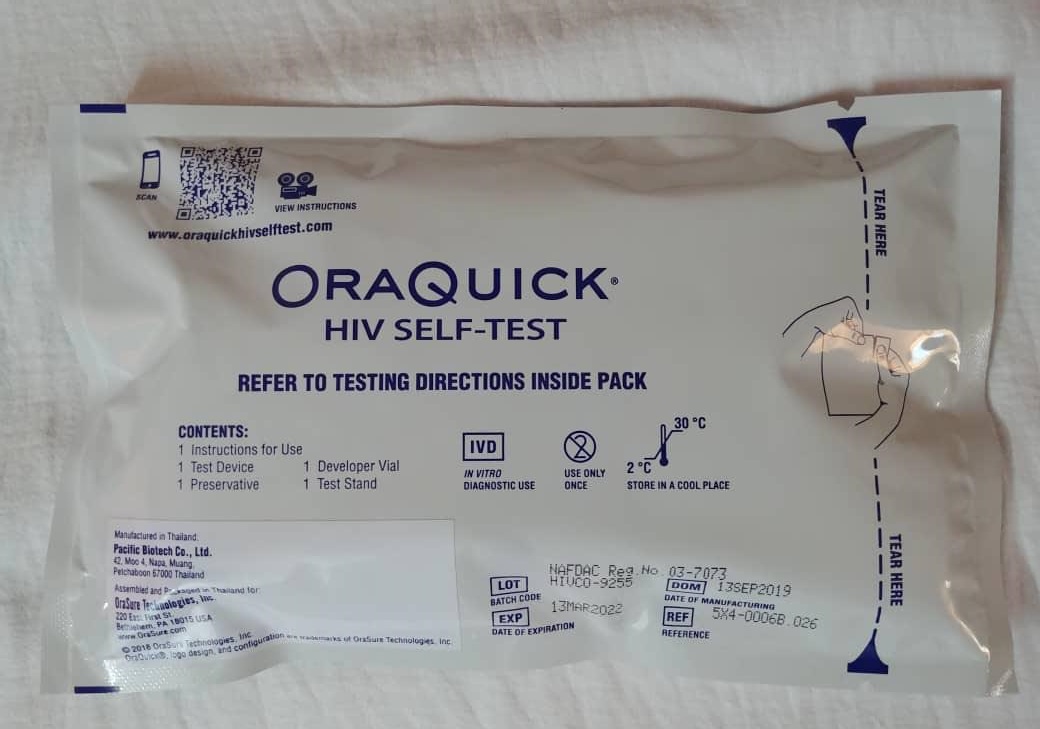
A total of 399 pregnant women and 238 male partners were randomly selected and enrolled in the HIV Self-Testing trial. In this study, researchers deployed an OraQuick, an oral fluid-based HIV self-testing kit, that aids one to check for HIV-1 and HIV-2 antibodies with results in 20 minutes.

Each pregnant woman was given two kits; for herself and her male partner in addition to HIV self-testing demonstrations, detailed pictorial instructions on how to use them. The study also made comparisons on understanding and following of HIV Self-Testing instructions by age and education level.
It was discovered that generally, both men and women understood self-testing instructions at 98%, although men said they needed pretest counseling.
“Partners' understanding of the HIV Self-Testing instructions did not vary by education level, but 4.4% of women with primary education reported difficulty in understanding HIV Self-Testing instructions compared with those with secondary and university education,” says study results.
Men (26.5%) were nearly twice as likely as women (16.0%) to report that they needed pre-test counseling before they performed HIV self-testing. Dr. Joseph KB Matovu, a Senior Research Associate at Makerere University School of Public Health, attributes this to men’s apparent lack of trust in the ability of HIV self-test kits to yield “true” results (some men doubt how this ‘saliva-based’ kit can show that one has HIV when HIV is found in blood; not in saliva) coupled with the uncertainty of how to handle HIV-positive results if they turned out to be HIV-positive.
“Pre-test counseling would help to prepare men for the type of HIV results that they might receive and help them to become emotionally ready to deal with any results that they may get,” says Dr. Matovu
Dr. Matovu, who is also one of the study investigators, further explains that men always fear to test for HIV preferring to wait for their female partners’ HIV test results; a situation known as proxy HIV testing. As a result of this mistaken belief, men believe that if their female partner is HIV-negative, they are also HIV-negative, yet sometimes this might not be the case.
Evidence from prior studies show that sometimes a woman might be HIV-negative when her male partner is HIV-positive or vice versa. This condition is known as HIV-discordance and is found in about 5-11% of couples tested in Uganda.
“It is, therefore, important that men are encouraged to test for HIV even if they know their female partners’ HIV test results; and, as our findings show, use of HIV self-testing, if preceded with pre-test counseling, can help to increase the percentage of men who know their HIV test results,” he adds.
In September 2019, the Government of Uganda launched an oral HIV self-test kit, with a view of empowering citizens especially men to embrace HIV testing. The initiative hopped to reduce new HIV/AIDs infections by 2020. OraQuick HIV self-test is a product of Orasure technologies, a U.S based medical device industry.
The 2017 Uganda Population-based HIV Impact Assessment (UPHIA) indicates that there are fewer men than women who have taken an HIV test in Uganda.
Although this is not a uniquely Ugandan issue, there is a growing worry that men usually take an HIV test when they are already symptomatic with AIDS, which limits their chances of survival as they start taking the treatment in the later stages of HIV infection.
The reason for the low uptake of HIV testing services among men is largely attributed to perceived fears of breach of confidentiality and associated stigmatization.
Others think that men perceive HIV clinics as spaces for women, while others fear challenges associated with reputational masculinity as well the perceived judgmental attitude of female health workers.
The government has increasingly advocated for the use of HIV self-testing kits as a way of increasing the numbers of individuals who test for HIV.
In this study, however, researchers say, if male confidence is boosted, they can support the national targets of having more men access the testing services and support timely interventions.
Uganda’s HIV testing services policy stresses the country’s desire to end the HIV epidemic as well as meeting the new nationally adopted global 95-95-95 targets towards the elimination of HIV by 2030, enshrined in the National HIV/AIDS Strategic Plan 2020/21-2024/25.
The study was conducted by a team of researchers from Makerere University School of Public Health (Dr. Kisa Rose, Dr. Joseph KB Matovu, Dr. Esther Buregyeya, Dr. Joseph Kagaayi, and Professor Rhoda Wanyenze); the Medical University of South Carolina (Dr. Caroline Vrana-Diaz, Dr. Angela M Malek and Dr. Jeffrey Korte); Mildmay Uganda (Harriet Chemusto [may her soul rest in peace], William Musoke, and Semei Christopher Mukama), and the Ugandan Ministry of Health (Dr. Shaban Mugerwa).
Written by Judith Grace Amoit & Davidson Ndyabahika

