By John Okeya
The seven fellows are part of the inaugural 2023 cohort of the Infection Prevention and Control (IPC) Program, a yearlong fellowship training offered by Makerere University School of Public Health (MakSPH) in collaboration with Uganda’s Ministry of Health (MoH), supported by the generous funding from U.S. Centers for Disease Control and Prevention (CDC).
Since 2023, these fellows have engaged in extensive and immersive training to enhance their expertise and bolster their capacities in developing strategies to prevent and manage infections within healthcare facilities across Uganda. Their goal has been to ensure patient safety, safeguard healthcare workers, and mitigate the significant risk of infection spread.
Uganda’s health system continues to grapple with substantial infection risks, primarily attributed to elevated rates of healthcare-associated infections (HAIs), which are infections patients can acquire while receiving medical treatment in health facilities like hospitals, clinics or nursing homes, or healthcare workers could acquire while administering treatment to patients.
Dr. Henry Kajumbula, the course facilitator and Program Lead for the MakSPH-IPC fellowship, highlighted these pressing concerns, noting that the infections are caused by bacteria, viruses, fungi and other pathogens, and may develop as a result of invasive procedures, the use of medical devices, or exposure to healthcare personnel or other patients carrying infectious agents. The examples, he said, are surgical site infections, bloodstream infections, urinary tract infections, pneumonia, and gastrointestinal infections.

Preventing healthcare associated infections remains critical, as this is essential towards ensuring patient safety and reducing the burden on healthcare systems, and prevent other risks relating to compromised patient safety, potential outbreaks of infectious diseases, escalated healthcare expenses due to treating avoidable infections, and the emergence of antibiotic-resistant pathogens or even death in certain incidents.
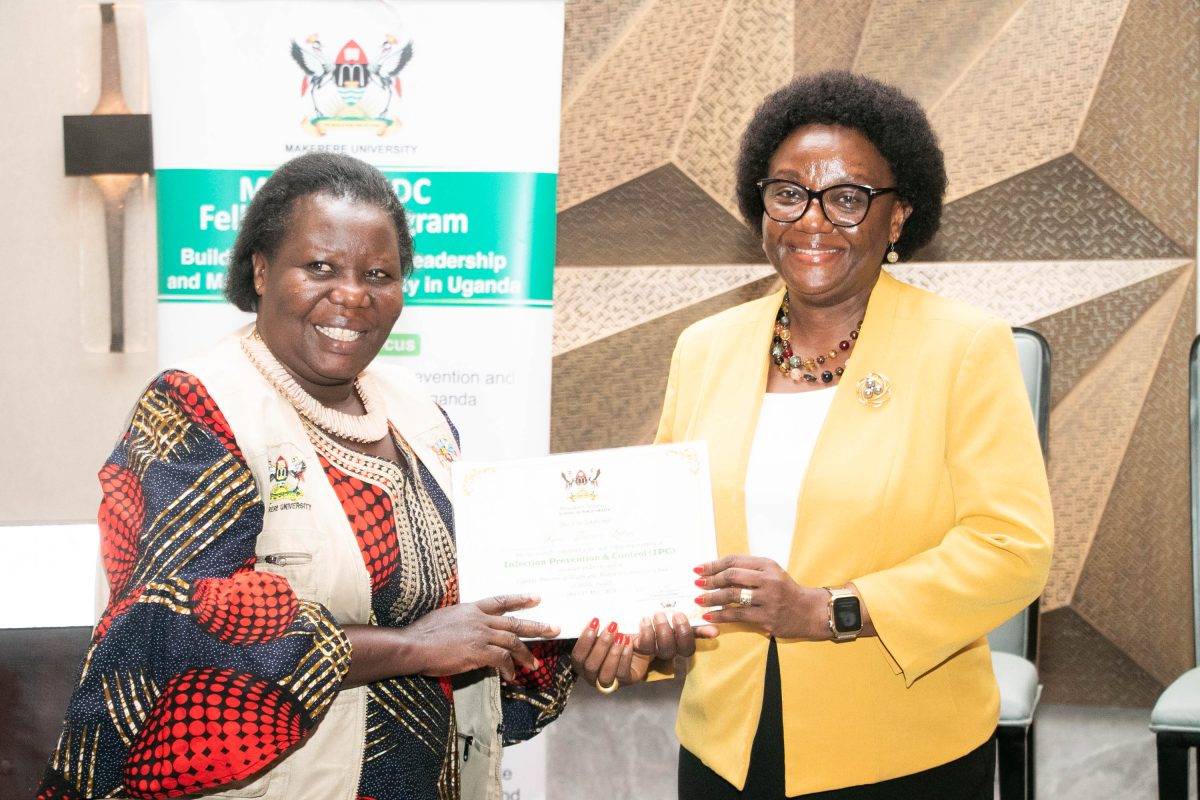
To confront these healthcare challenges, the fellows, as part of their training, devised and executed programs aimed at infection prevention and control within various healthcare facilities in Uganda. They showcased their initiatives during their graduation before receiving certificates during the event organized at Four Points by Sheraton in Kampala, on May 23, 2024.
Among the different initiatives, Ms. Grace Musiimire’s innovation emerged the overall best, bagging the award for the best innovation for the first cohort of the program. Grace, an Assistant Nurse Officer at Mengo Hospital in Kampala – where she has worked for now close to a decade, focused her fellowship project on improving compliance with medical waste segregation protocols among healthcare workers at her health facility in Mengo.
“Waste segregation is the core of waste management and should be done at the source of generation. At Mengo Hospital, waste segregation practices were as low as 31 percent according to my baseline. This project sought to improve compliance with medical waste segregation protocols among healthcare workers from 31 percent in October 2023 to 60 percent by the end of March 2024,” Grace noted during her presentation.
Through her initiative, Grace established a project committee together with colleagues at Mengo Hospital, conducted mentorship sessions, and raised awareness among staff, through which she was able register an improvement of waste segregation by 69 percent within the public health facility by March 2024 following supervision, accountability, and continuous monitoring.
From her observation, waste segregation, a process of separating different types of waste materials into distinct categories to enable more effective and efficient waste management practices, including recycling, reuse, treatment, and disposal, is key towards improving infection prevention and control, urging for the need to scale up the project to all the units within Mengo Hospital and implementing feedback mechanisms to monitor compliance for maximum impact.
Her colleague, Ms. Harriet Kembabazi, a Principal Nursing Officer at the Ministry of Health with a degree in nursing and one of the beneficiaries of the program, said lacking formal IPC training propelled her to pursue this fellowship. She was among the over 450 initial applicants, from whom seven fellows were selected, for the first cohort of the IPC fellowship at MakSPH.
“I extend our sincere appreciation. It has been a transforming experience, the fellowship gave us an opportunity to interact with highly skilled professionals, who have taken us through important sessions in IPC and beyond. We have gained important skills that we feel will support in strengthening our healthcare system in Uganda,” Harriet said, with gratitude.

“With this deeper knowledge, I envision contributing to Uganda’s evolving IPC program, which is poised to become an integral part of the healthcare system following recent epidemics. My goals are to develop as an IPC expert, provide mentorship, and ensure quality improvement in critical areas like waste segregation. This fellowship equipped me to make lasting impacts in IPC policy, capacity building, and sustainable healthcare delivery,” Harriet further noted.
Kembabazi felt the program was timely. CDC, MoH, and Makerere University enabled the training, she said, further noting that the inaugural cohort, met their expectations for IPC. The fellows want the Program expanded to benefit additional healthcare workers in Uganda, and receive continuing supervision and coaching to scale their inventions.
MakSPH has developed a diploma in Infection Prevention and Control, a course currently awaiting accreditation from the National Council for Higher Education (NCHE), to fill the void in IPC training in Uganda. Prof. Rhoda Wanyenze, the Dean MakSPH, during the graduation of the fellows, resounded the need to develop a critical mass of IPC professionals to deliver Uganda’s public health needs.
“IPC is such an important area and yet we don’t speak about it enough. Just imagine when you contact a healthcare facility, you could leave with a disease you never came with that you could even die from. Many have died because of this, because of infections they pick when they contact the facility, which is probably worse than what they came with,” said Prof. Wanyenze.
The Dean revealed the urgent need to raise consciousness and awareness around IPC practices in Uganda “starting with the training of IPC professionals.” She recognized all the partners who supported the fellowship to make the dreams of the seven graduates in IPC fellowship a reality, extending special gratitude to the Ministry of Health for walking the journey and the CDC – a long term partner of the School, for their dedicated funding.
Dr. Kimberly McKinney, a CDC Epidemiologist, during the graduation, noted that strong IPC practices can prevent infection and their spread, however to be effective, she said there must be strong support from the facility leadership.
Dr. Kimberly encouraged the graduates to be future leaders in IPC at their different facilities, joining her colleague, Dr. Janelle Kibler, also an Epidemiologist and EIS Officer under the CDC International Infection Control Branch to request the MakSPH IPC fellows to put their skills in improving population health in Uganda.

“Infection prevention and control practices, when done well, lead to the absence of illness, morbidity, and mortality. This makes our work, and the reason we do it, complex and difficult. What we are fighting is always invisible and requires that we and all the healthcare staff rethink the things we have been doing every day. So, as you take this great accomplishment forward in your working life, I urge you not to forget this fight that we are fighting,” Dr. Janelle Kibler.

“IPC should not be something we do only when we have Ebola or Covid-19. Let’s institutionalize it, and we all have a task to make sure this happens. That is my appeal to all of us. Let’s keep going and let’s shift the terrain so that we can protect more people and so that we ourselves are not victims of poor IPC practices within the spaces that we interface with,” Prof. Wanyenze.
| Attachment | Size |
|---|---|
| abstract_book (10.85 MB) | 10.85 MB |