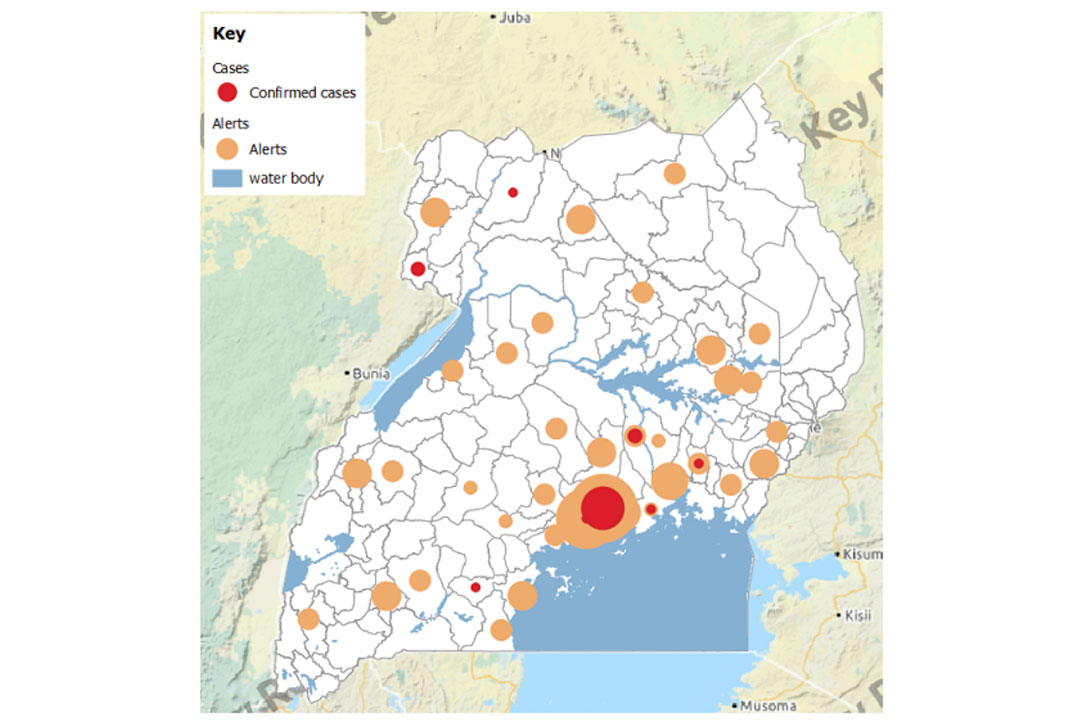
As of March 25, the number of COVID19 cases had risen to 14 in Uganda less than a week since the first case was identified on March 20 as the viral infection continues to wreak havoc around the world.
As the country under the stewardship of the Health ministry continues to put in place measures to control the spread of the disease some challenges abound. There have been reports that some people who are under quarantine switch off their phones making follow up hard while others are not following quarantine orders.
Amidst this confusion especially among the suspected cases and their families, efforts need to be made to reach out through all possible means to establish why these people are behaving the way they are.
We need to hear from them and therefore respond appropriately. I don’t know how the quarantine for COVID-19 is being done in Uganda but would like to take this opportunity to share our West Africa (Sierra Leone) Ebola Virus Disease (EVD) experience and we can pick a lesson or two from it.
We made quarantine process very humane.
- We prepared the community including the suspected case(s)/person(s) on why we were carrying out the quarantine. We informed them that ALL of us (the suspected case(s), the community and the surveillance team/response team) had a role to play. The role(s) each party MUST be clearly spelt out.
- Given that we were putting suspected case(s) under quarantine for 21 days (for the case of Ebola Virus Disease), we provided basic amenities (food and charcoal, hygiene-related utilities-chlorine tablets, chlorine buckets and trained them how to mix the chlorine by themselves). For the COVID 19 scenario, the task force/government needs to think about what form of basic amenities/support to provide to the suspected case(s) during the quarantine period.
- In a scenario where suspected case(s) were uncooperative;
- We moved them to an agreed venue/premises outside their homes like public spaces like schools. We quarantined the uncooperative suspected case(s) in such premises/venue for 21 days, BUT in the event that the suspected case(s) becomes symptomatic before the 21 days, then he/she would be re-located to the holding centre for screening for EVD.
- The Ebola response provided basic needs (food and hygiene related utilities like-buckets, soap, chlorine tablets etc) to the suspected cases. These were mobilized from government and partners involved in the EVD response.
- We ensured that security Police/Army was provided for the entire quarantine period to restrict movement of the suspected case(s) but as well for their safety.
- Provided a register for capture of information any of the visitors (Names, addresses and the reason of visiting
- We sensitized the suspected case(s) on the DOs and DON’T’s during the quarantine period. For COVID-19 the suspected case(s) follow the MoH developed information on DO’S AND DON’TS ON CORONAVIRUS DISEASE.
- We talked to the suspected case(s) including their families on a daily basis, to address their fears/concerns.
So, in summary to ease the COVID 19 surveillance especially among the uncooperative suspected cases (those who are under quarantine BUT switch off their phones/don't follow the quarantine orders) for that matter, Uganda could consider:
- Identify space such Public Schools to accommodate such suspected case(s)
- Provide security (Police/Army) to restrict their movement as well as safety during the quarantine period (14 days). The security MUST be permanently stationed in the agreed premises/venue.
- Provide basic needs-food-(WFP - World Food Programme, OPM - Office of the Prime Minister) and hygienic related amenities soap, disinfectants, drinking water etc. during the 14 days.
To conclude, the above MUST apply to the suspected cases who fail to adhere to the quarantine procedures.
*The author is Samuel Etajak, a lecturer at the Makerere University School of Public Health and participated in the Ebola Virus Disease response in West Africa.

