
By Carol Esther Nabbanja and Michael Obeng Brown
The Nottingham Trent University and Makerere University (NTU-Mak) Partnership has intensified efforts to strengthen antimicrobial stewardship in Nakaseke and Butambala, tackling the growing public health need to combat rising drug-resistant diseases through “One Health”.
One Health is a globally recognised approach that highlights the interconnectedness of humans, animals, and the environment. Originating from the understanding that diseases can be transmitted between animals and humans and are influenced by environmental factors, this model underscores the need for collaborative solutions to address public health threats.
One such threat is antimicrobial resistance (AMR) — a condition where disease-causing organisms like bacteria, viruses, fungi, or parasites evolve to resist known effective medications. This is highly prevalent in Uganda and around the globe, making infections harder to treat and increasing the risks of further disease spread, severe illness, or death.
In a bid to bolster global efforts in promoting antimicrobial stewardship — meaning the responsible and effective use of antibiotics and other antimicrobial drugs to ensure they remain effective in treating infections and preventing the development of drug-resistant pathogens (disease-causing organisms) — the NTU-Mak Partnership recently concluded a weeklong training workshop in May 2024, in Butambala and Nakaseke districts, Central Uganda.
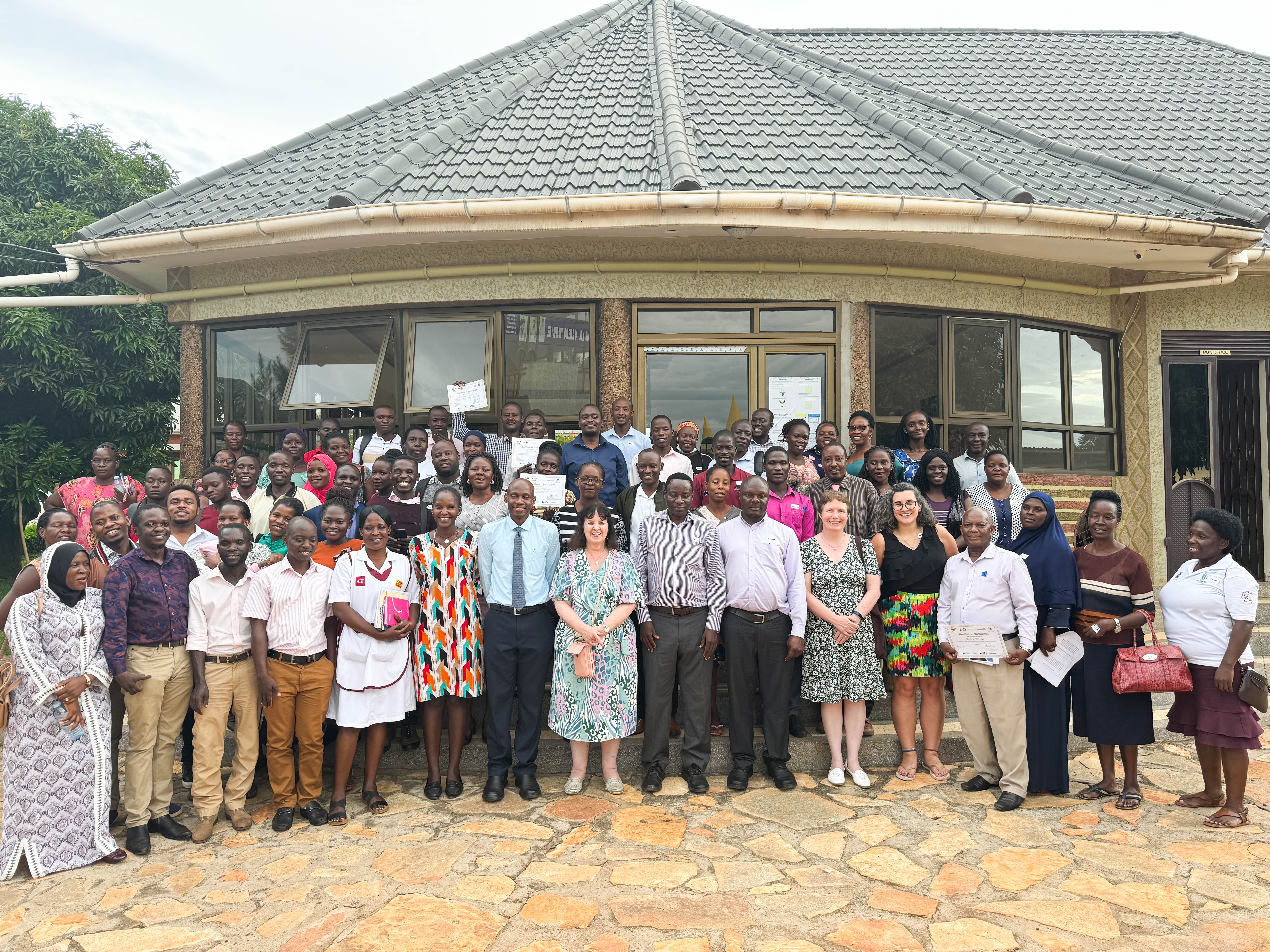
The training equipped over 120 healthcare professionals with essential knowledge and skills for effective antimicrobial management and prescription, including nurses, doctors, pharmacists, veterinarians, and environmental health experts. Facilitated by experts from the UK and Uganda, the event fostered cross-cultural learning between the Global North and South.
The training was done under the NTU-Mak project titled Centre of Excellence for Antimicrobial Stewardship in Central Uganda, supported by the Commonwealth Partnerships for Antimicrobial Stewardship Scheme (CwPAMS) - a health partnership programme and initiative of the Commonwealth Pharmacists Association (CPA) and the Tropical Health and Education Trust (THET) under the UK Aid Fleming Fund at the Department of Health and Social Care (DHSC), which seeks to strengthen health systems in Uganda and the region.
The comprehensive training, conducted in collaboration with Buckinghamshire Healthcare NHS Trust (BHT), Entebbe Regional Referral Hospital, Uganda’s Ministry of Health (MoH), and the local governments of Butambala and Nakaseke districts, focused on enhancing participants' knowledge of antimicrobial resistance, antimicrobial stewardship, Infection Prevention and Control (IPC), and substandard and falsified medicines (SFMs). SFMs are medical products produced in poor and unhygienic conditions by unqualified personnel, often containing unknown impurities and sometimes contaminated with bacteria.

According to World Health Organization (WHO) reports, the rising trend of antimicrobial resistance is complicating treatment and facilitating the spread of more resilient and dangerous infections, including tuberculosis (TB), malaria, HIV, pneumonia, and gonorrhoea.
The burden of antimicrobial resistance remains pronounced. According to the statistics from the Institute for Health Metrics and Evaluation (IHME), globally, at least 4.95 million people died in 2019 due to drug-resistant infections, with antimicrobial resistance directly responsible for 1.27 million deaths, of which one in five occurred among children under five.
The report confirms that Uganda had 7,100 deaths directly attributed to antimicrobial resistance and other associated 30,700 deaths within the same year, 2019, with the country ranking as the 165th highest in age-standardized mortality rate per 100,000 population associated with antimicrobial resistance across 204 countries evaluated.
What is telling, the IHME report notes that deaths caused by antimicrobial resistance alone in Uganda comparatively exceed those from respiratory infections, tuberculosis, cardiovascular diseases, HIV/AIDS, sexually transmitted infections, neglected tropical diseases, malaria, and neoplasms (abnormal and excessive growth of tissue).
The leading pathogens (microorganisms, such as bacteria, viruses, fungi, or parasites, that can cause disease in their host) identified in Uganda include Klebsiella pneumoniae, Streptococcus pneumoniae, Escherichia coli, Staphylococcus aureus, and Salmonella Typhi. These microorganisms are said to be primarily responsible for causing lower respiratory infections, bloodstream infections, and peritoneal and intra-abdominal infections.
Although antimicrobial resistance cannot be eradicated, research shows it can be effectively slowed and contained. To address this challenge, Uganda adopted the Antimicrobial Resistance National Action Plan 2018-2023, emphasizing health education as a crucial strategy for promoting responsible antibiotic use.
The Action Plan outlines a coordinated and collaborative One Health approach involving key stakeholders from government and various sectors to tackle the threat of antimicrobial resistance. The NTU-Mak Partnership, through its long-term work in Central Uganda, has continued to significantly contribute to strengthening health systems, addressing public health risks, and improving health outcomes for the local communities.
During the recently concluded training, Dr. Jody Winter from NTU introduced antimicrobial resistance, stressing the urgent need for global action. She encouraged participants to “think globally but act locally,” a message reinforced by practical demonstrations. These included the Building Blocks to Modern Medicine and the Balloon experiment, both of which illustrated the worldwide impact of antimicrobial resistance and its specific implications for Uganda.
Meanwhile, Natasha Hamilton, a pharmacist at Buckinghamshire Healthcare NHS Trust, led engaging group discussions on antimicrobial stewardship, challenging participants with thought-provoking questions about antimicrobial resistance and stewardship. These discussions emphasized the need for better awareness, hand hygiene, compliance with prescribed dosages, pharmacovigilance, and the enforcement of policies and regulations on antibiotic use.
Gender Equality and Social Inclusion (GESI) was also a significant focus of these workshops. Facilitated by Elma Banyen and Michael Obeng Brown, PhD candidates at NTU, this session reminded participants of the need to consider gender inclusion in their health service delivery, aiming to eliminate harmful inequalities at health centres and within communities.
Dr. Jean O’Driscoll from BHT and Filimin Niyongabo from Makerere University led discussions on reducing cross-infections, stressing the importance of hand hygiene and the links between environment, host, and pathogen through the Epidemiological Triad. Dr. Herbert Bush Aguma from Makerere University’s Department of Pharmacy educated participants on identifying substandard and falsified medicines, while Prof. Lawrence Mugisha, also from Makerere introduced the One Health approach, emphasising its importance in combating antimicrobial resistance, particularly in infection prevention, vaccination, and proper nutrition for animals.
Dr. Lawrence Kisuule, the District Veterinary Officer of Nakaseke, shared ongoing interventions to fight antimicrobial resistance, including staffing at all levels, profiling private veterinary practitioners, and inspecting veterinary drug shops and clinics while highlighting the need for collective action to combat antimicrobial resistance in Uganda.
Dr. David Musoke, the NTU-Mak Partnership Co-Principal Investigator at Makerere joined his colleague, Prof. Linda Gibson, the Co-Principal Investigator at Nottingham Trent University (NTU) to thank all collaborators of the project. Dr. Musoke also encouraged the participants, who were awarded certificates upon completion of the training, to apply their knowledge gained in promoting antimicrobial stewardship for the safety of humans, animals and the natural ecosystem.


