
A new study in Uganda has shown a significant increase in oxygen access and pulse oximetry among neonates and children in health facilities.
Preliminary findings published in The Lancet, the world's highest-impact medical and academic journal show the positive impact of a diverse oxygen systems strengthening intervention on diagnosis, oxygen therapy use, and mortality rates.
Titled; “Improving Effective Coverage of Medical Oxygen Services for Neonates and Children in Health Facilities in Uganda: A Before-After Interventional Study,” the study shows that large-scale improvements in hospital oxygen services are achievable in a relatively short timeframe and have great potential for impact.
The study was led by Dr. Freddie Ssengooba, an Associate Professor of Health Policy Planning and Management, at the School of Public Health and Dr. Freddy Eric Kitutu, a Senior Lecturer of Health Systems Pharmacy both co-chairs of the Lancet Global Health Commission on Medical Security. Other researchers on the study include Hamish Graham from the University of Melbourne, Yewande Kamuntu, Blasio Kunihira, Santa Engol, Jasmine Miller, Absolom Zisanhi, Dorcas Kemigisha, Lorraine Kabunga and Felix Lam all from Clinton Health Access Initiative, Dr. Charles Olaro from Uganda's Ministry of Health and Dr. Harriet Ajilong from the Uganda Paediatric Association.
From June 2020 to June 2022, an intervention study assessed neonates and children at 31 government health facilities in Uganda's Busoga and North Buganda regions, located at altitudes of 1100-1400 meters. The primary outcome measured the proportion of patients with documented pulse oximetry on admission.
Secondary outcomes included patients with severe hypoxaemia (SpO2 < 90%) receiving oxygen, overall oxygen usage, and appropriate oxygen usage. The study's primary effectiveness analysis compared pulse oximetry coverage before and after the intervention, incorporating a 4-month washout period. The analysis utilized mixed-effects logistic regression, adjusting for clustering at individual facilities, age (child versus neonate), and sex (male versus female).
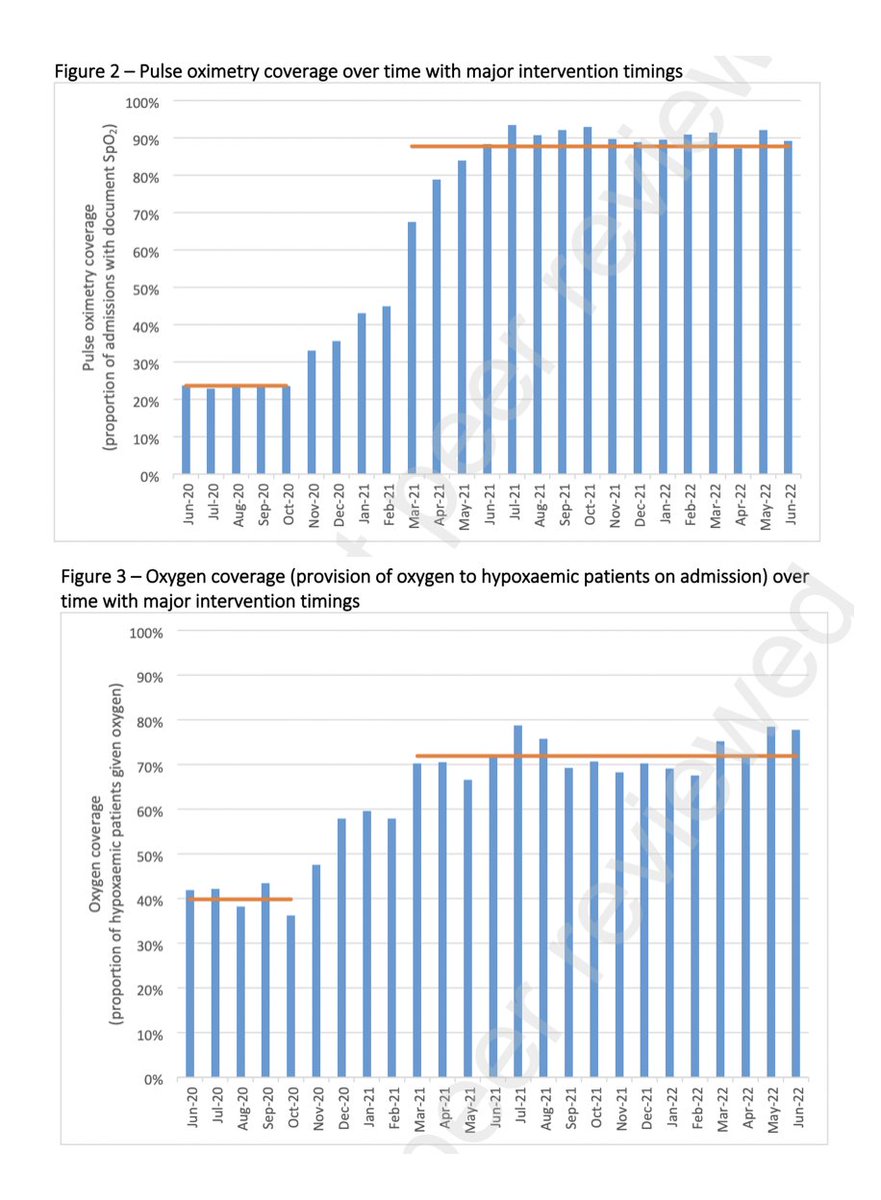
Researchers analyzed 64,562 patients (25% neonates) and observed a significant rise in pulse oximetry coverage during the intervention period, increasing from 24% to 88% with an adjusted odds ratio of 40.1 (95% confidence interval: 37.4 to 42.9).
They also observed better oxygen coverage for children and neonates with low oxygen levels, increasing from 40% to 71%, with an adjusted odds ratio of 3.81 (95% confidence interval: 3.26 to 4.46).
Additionally, there was a slight increase in overall oxygen usage, rising from 8% to 11%, with an adjusted odds ratio of 1.95 (95% confidence interval: 1.79 to 2.13).
“Improvements were relatively greater in smaller facilities and for children (versus neonates). We estimated additional patients served and lives saved in the post-intervention period using observed effect estimates in this and other studies,” reads the study.
With these findings, researchers are calling on governments in low-income and middle-income countries to create oxygen plans and invest in proven solutions, like incorporating pulse oximetry in regular hospital care, and providing clinical as well as biomedical mentorship and support.
For all age groups, medical oxygen is essential for both acute and chronic health problems. Scientific evidence suggests access to medical oxygen services that are safe, economical, and appropriate is essential for improving overall health and achieving Sustainable Development Goals. Unfortunately, inadequate or inconsistent oxygen supplies present challenges for many low- and middle-income nations, particularly for small medical facilities in underserved areas.

Disruptions in the oxygen supply during the COVID-19 pandemic caused excessive deaths, which predominantly affected countries with low to middle incomes. According to a 2021 study, half of the COVID-19 patients who died in 64 critical care units across ten African countries did not receive the required medical oxygen.
The study was funded by a grant from the Bill and Melinda Gates Foundation (BMGF) and ELMA Philanthropies to the Clinton Health Access Initiative (CHAI) and approval from Makerere University School of Health Sciences Research and Ethics Committee, and the Uganda National Council of Science and Technology.
Available at SSRN: https://ssrn.com/abstract=4676954 or http://dx.doi.org/10.2139/ssrn.4676954
By Davidson Ndyabahika

